Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Diagnostic Therapeutic Attitude in Patello Femoral Instability
*Corresponding author:Enrique González García, Traumatology and Orthopedic Surgery Service, Burgos University Hospital, Spain
Received: May 17, 2022; Published:June 03, 2022
DOI: 10.34297/AJBSR.2022.16.002238
Case Report
The Patellofemoral Instability (PFI) is the tendency to dislocation or subluxation, frequent, symptomatic, of the Patellofemoral Joint (PFJ).
With the anamnesis and exploration, we must differentiate
between two situations that can occur exclusively or concomitantly:
a. Instability is the impression of imminent dislocation that the
patient feels when, with the knee between 0˚-30˚ of extension
and the quadriceps relaxed, displacement is forced in patella
lateral direction [1,2]. The “dynamic apprehension sign” [3]
consists of the “relief of the imminent sensation of dislocation
when it is stopped simultaneously with the pressure on the
external side while pushing outwards and distally from the
internal” which has 100% sensitivity and 88.4% specificity
regarding dislocation under anaesthesia, which is the sure sign
of instability.
b. Patellar mal tracking is the medialization movement of the
patella in the first degrees of flexion, it is pronounced, abrupt,
greater than 4mm, it is called the “J sign”, it is a characteristic
sign of malalignment, although not pathognomonic [4,5].
In Order to Consider Its Pathogenesis and Its Diagnostic Approach, The Following Classification is Proposed [6]:
Type 1: No instability or patellar malt racking.
Type 2: Pure instability due to rupture of the medial patellofemoral ligament (mpfl) [7] without malalignment.
Type 3: Concomitance of instability and patellofemoral mal
tracking:
a. Functional imbalance between the weakness of the vastus
obliquus medialis and the retraction of the external lateral
retinaculum, which produces “inclination” identifiable with
the Kolowich sign or “tilt test”: The impossibility of manually
placing the patella horizontally if the quadriceps is relaxed
[7].
b. Patella alta was defined by Caton and Deschamps [8] by
an index (CDI≥1.3) measured by a knee X-ray in pure
lateral projection. There is also another parameter for the
radiological diagnosis of this risk factor, called “Biedert
patellotrochlear index <12.5% [9]”, which is obtained by
MRI.
c. Increased valgus vector defined by CT when the “tubercletrochlear
groove” TT-TG distance >20mm [1], or by MRI in
which the same measurement is 2-4mm less [3,8].
d. Genu valgum measured by simple posteroanterior
radiography of the entire lower limb with the patient
standing, which if >5˚ must be corrected surgically in the
presence of PFI [10].
e. Rotational alterations: either an increase in Femoral
Anteversion (FAV) should be suspected through the Staheli
maneuver [11], and External Tibial Rotation (ETR) because
the “thigh foot angle” angle is greater than the Foot Angle
Progression (FAP), that is >15˚. Normal values of FAV and
ETR are established by CT at 14˚ SD=7˚, and 25˚ SD=7˚
respectively [12]. The malrotation correction criterion is
given by the presence of PFI with FAV>35˚ and ETR >45˚
[6,13].
Type 4:Instability and proximal malalignment due to severe Trochlear Dysplasia (TD), which are Dejour types B and D, identifiable on an X-ray pure sagittal profile plain if supratrochlear prominence or “spur” is observed; is not essential but it is advisable to corroborate by CT or MRI [14,15].
Type 5:There are patients who have not subjective sensation of instability but have patellar mal tracking throughout the entire flexion-extension of the knee. In the simple inspection of the patient in standing position, it is observed how the knees “look inward”, a sign described as ‘’in wardly pointing knee’’ [16,17]. This complete loss of patellar alignment is due in 60% of cases to severe alterations rotational, and in the other 40% to severe hypoplasia of the medial femoral condyle associated with type C or D of trochlear dysplasia, all of them, with very prolonged symptoms of PFI over time [6].
Therapeutic Attitude: It Must Follow the Following Criteria
Conservative treatment
It is usually recommended when there has only been a single episode of patellofemoral dislocation [18] and consists of strengthening the vastus medialis and the use of specific orthoses in addition to proprioceptive training, together with the avoidance of risky activities such as jumps, turns or sudden decelerations of the race.
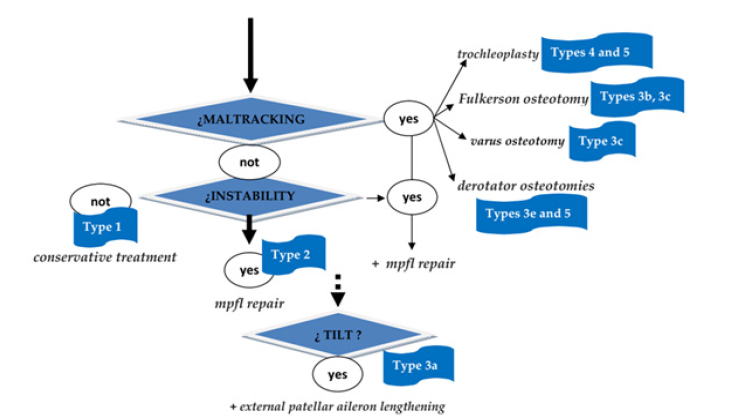
It is performed if previous conservative treatment, tried for several months, fails, or after repeated episodes of dislocation. In the first place, restore the alignment attending to the factors that alter it (DT, patella alta, valgus vector, FAV/ETR) by implementing of trochleoplasty, distalization of the anterior tibial tuberosity, Fulkerson osteotomy, derotator osteotomies of the femur or tibia, depending on the anatomical cause of malalignment. The use of trochleoplasty in non-expert hands is highly controversial and it is possible that tibial tuberosity osteotomies may be indicated in the treatment of DT4. Repair of the medial patellofemoral ligament is indicated to restore instability, once the alignment has been corrected, but never. Finally, the correction of the inclination is decided intraoperatively if the previous techniques have been conducted, its intra-surgical persistence [19] is demonstrated by observing the turning in the first 20˚ of flexion. It is contraindicated [13] to conduct the isolated correction of the inclination with section of the external patellar aileron or its lengthening in “z” [20]. In outline, the surgical protocol follows the following scheme (Figure 1).
References
- Fairbank HA (1937) Internal Derangement of the Knee in Children and Adolescents: (Section of Orthopaedics). Proc R Soc Med 30(4): 427-432.
- Smillie IS (1951) Internal derangements of the knee joint. Br Med J 2(4735): 841-845.
- Post WR, Fithian DC (2018) Patellofemoral Instability: A Consensus Statement From the AOSSM/PFF Patellofemoral Instability Workshop. Orthop J Sports Med 6(1): 2325967117750352.
- Post WR (1999) Clinical evaluation of patients with patellofemoral disorders. Arthroscopy 15(8): 841-851.
- Sheehan FT, Derasari A, Fine KM, Brindle TJ, Alter KE (2010) Q-angle and J-sign: indicative of mal tracking subgroups in patellofemoral pain. Clin Orthop Relat Res 468(1): 266-275.
- Frosch KH, Schmeling A (2016) A new classification system of patellar instability and patellar mal tracking. Arch Orthop Trauma Surg 136(4): 485-497.
- Tanner SM, Garth WP Jr, Soileau R, Lemons JE (2003) A modified test for patellar instability: the biomechanical basis. Clin J Sport Med 13(6): 327-338.
- Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H (1982) Low kneecaps. Apropos of 128 observations [Patella infera. About 128 cases]. Rev Chir Orthop Restorative Appar Mot 68(5): 317-325.
- Biedert RM, Albrecht S (2006) The patellotrochlear index: a new index for assessing patellar height. Knee Surg Sports Traumatol Arthrosc 14(8): 707-712.
- Swarup I, Elattar O, Rozbruch SR (2017) Patellar instability treated with distal femoral osteotomy. Knee 24(3): 608-614.
- Staheli LT, Corbett M, Wyss C, King H (1985) Lower-extremity rotational problems in children. Normal values to guide management. J Bone Joint Surg Am 67(1): 39-47.
- Solano A, Brill Kremer W, Tey Pons M, Espiga Tugas X (2000) Normal alignment of the lower extremities in the adult. Torsional misalignments of the lower extremities. Clinic Opathological implications. Monographs SECOT 2 J Ballester First edition. Barcelona: Mason 11-16.
- Sanchis Alfonso V (2016) How to Deal with Chronic Patellar Instability: What Does the Literature Tell Us? Sports Health 8(1): 86-90.
- Dejour H, Walch G, Nove Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2(1): 19-26.
- Dejour D, Le Coultre B (2007) Osteotomies in patello-femoral instabilities. Sports Med Arthrosc Rev Mar 15(1): 39-46.
- Cooke TD, Price N, Fisher B, Hedden D (1990) The inwardly pointing knee. An unrecognized problem of external rotational malalignment. Clin Orthop Relat Res (260): 56-60.
- Dickschas J, Harrer J, Pfefferkorn R, Strecker W (2012) Operative treatment of patellofemoral maltracking with torsional osteotomy. Arch Orthop Trauma Surg 132(3): 289-298.
- Jain NP, Khan N, Fithian DC (2011) A treatment algorithm for primary patellar dislocations. Sports Health 3(2): 170-174.
- Arendt EA (2012) Lateral-sided surgery with MPFL reconstruction: when is this needed? In: Bonnin M, Servien E, Demey G, Dejour D, eds. La Patella. Montpellier, France: Sau ramps Medical 2012: 119-123.
- Hinckel BB Arendt EA (2015) Lateral Retinaculum Lengthening or Release. Oper Tech Sports Med 23(2): 100-106. ns C, Lewis A L, et al. (2021). A mouse model displays host and bacterial strain differences in Aerococcus urinae urinary tract infection. Biology open 10(8): bio058931.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.